We use our resources to generate evidence, inform debate, and support innovation that advances social well-being. Our independence allows us to take the long view, addressing complex, long-term challenges where research can make the most significant difference.
Through our work, we aim to deepen understanding of today’s most pressing issues and help policymakers and practitioners apply evidence to improve outcomes. A focus on inequality, disadvantage and vulnerability runs through our work, shaping our priorities and the research we fund.
Here you can explore our strategic priorities, the research we support, and the impact of our work.
Our priorities
-
A prosperous and fair society
How can we build a prosperous and fair society, where people are secure and can fulfil their potential?
-
An inclusive society
How can we build an inclusive society, where people thrive and feel they belong, in the context of changing demography and ways of life?
-
Science, technology and society
How can we ensure that developments in science and technology work for people and society?
-
Climate change
How can policies to address climate change be developed in a way that promotes a prosperous, fair and inclusive society?
-
Trustworthy and effective institutions
How can we build and maintain the effective, accountable and trustworthy institutions that our society and democracy needs?
Read our Strategic Review
Our impact
-

- Impact
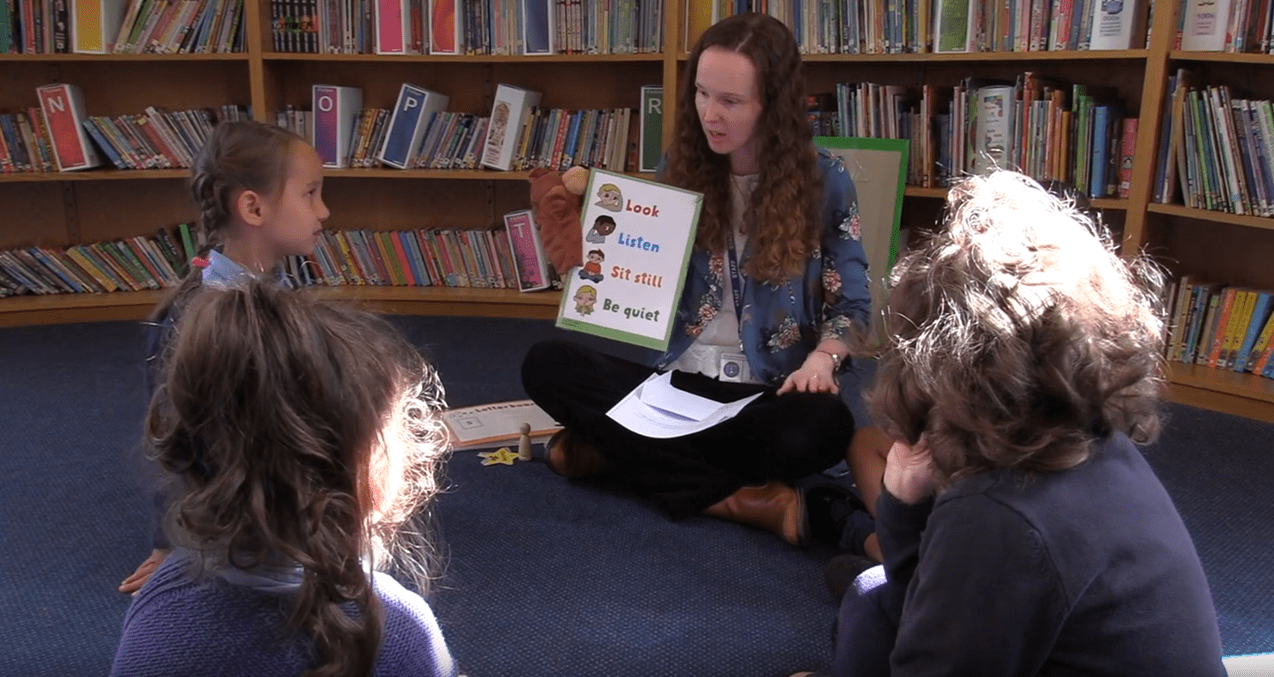
Nuffield Early Language Intervention in the making
NELI has been evaluated in robust trials and has been shown to improve children’s oral language.
-

- Impact
Helping divorcing couples to navigate pensions on divorce
We have funded research to help divorcing couples share their pensions more fairly, and...
-

- Impact
Addressing the social and economic impacts of the COVID-19 pandemic
Findings from our COVID-19 research projects have been influential in many policy discussions and together, offered a multifaceted perspective on the crisis.
Our programmes
-

- Programme
Grown up? Journeys to adulthood
Grown up? dives into how young people aged 14 to 24 are making the journey to adulthood - and what this means for policy, research and wider society.
-

- Programme
Public right to justice
Examining how the justice system serves the public and how it can better meet people's legal needs.
-
- Programme
Essays on philosophy in public life
-
We fund research that:
- Finds ways to improve educational outcomes through policy change and interventions that are grounded in robust evidence. Learn more about this area.
- Builds on our understanding of how people’s welfare, including their economic prosperity, health and participation in society, is shaped by different social, economic and technological factors. Explore these projects.
- Strengthens the justice system, making it more accessible, effective, and fair, especially for people facing disadvantage and the points where they encounter the system. Discover this work.